Blog
The average period comes every 28-30 days, lasts 3-6 days, and typically has 1-2 heavier flow days then tapers off. Every woman is different and blood flow pattern can change over time. Typically, earlier on in the adolescent and teenage years, periods can be heavier and last longer. Over time, this should lessen. But in many women, heavy menstrual bleeding continues throughout the reproductive years. While this is a common experience, heavy menstrual bleeding warrants a visit to your doctor, preferably a gynecologist. What is Heavy Menstrual Bleeding? The medical term for heavy menstrual bleeding is “menorrhagia”. Typically, it is recognized by taking note of how often you change a pad or tampon. If your flow causes you to need to change pads/tampons more than every 1-2 hours, you are soaking through your clothes, you require more than one pad at a time, or you bleed through even an extra long or super absorbency product overnight, you are experiencing heavy menstrual bleeding. Also, if your periods last more than 7 days, you have heavy menstrual bleeding. What Causes Heavy Menstrual Bleeding? The list of potential causes of heavy menstrual bleeding is long. Most are benign (non-cancerous) reasons such as ovulatory dysfunction from hormonal abnormalities, uterine fibroids or polyps, adenomyosis, infection, or bleeding disorders. Ovulatory Dysfunction Ovulatory dysfunction occurs when a woman does not ovulate (release an egg) regularly each month. This leads to thickening of the lining of the uterus and heavy periods when bleeding does occur. Ovulatory dysfunction is most common during adolescence when periods first start or perimenopause when periods are stopping. It can also occur with certain medical conditions such as hypothyroidism and polycystic ovarian syndrome (PCOS). Uterine Fibroids Fibroids are benign growths which develop within the muscle, inside, or on the surface the uterus. They are most common in African American and Latino women. The exact cause of fibroids is unknown. They can range in number and size and affect different women differently. For example, small fibroids (less than 3 centimeters) are typically asymptomatic and many women do not even know they have them. Contrastingly, in some women, fibroids grow very large (10 centimeters or greater) or many are present, and they cause symptoms such as heavy periods, bloating, painful sex, infertility, and even bladder/bowel problems. While fibroids are not dangerous, they can be quite bothersome. They grow in the presence of estrogen and thus can increase in size during the reproductive years and pregnancy and typically shrink after menopause. They are typically diagnosed by ultrasound.
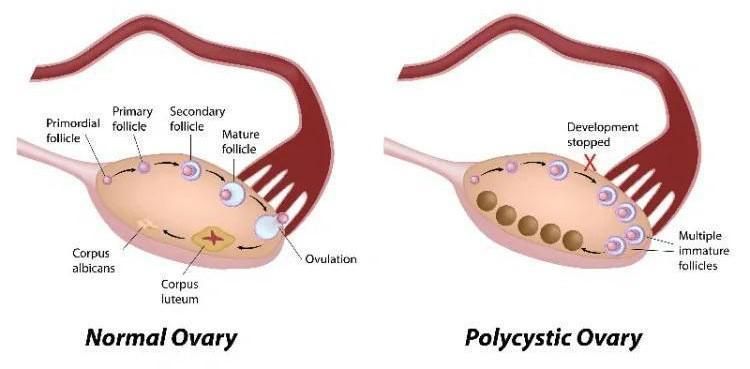
Polycystic Ovarian Syndrome, or PCOS, is a common condition which affects women of all reproductive ages. It typically is associated with multiple symptoms including: - irregular bleeding - heavy and prolonged bleeding - risk of uterine cancer - infertility - unwanted hair growth - obesity / difficulty losing weight WHAT IS NORMAL? Women have a uterus, 2 fallopian tubes, and 2 ovaries. The average woman has a 28-day menstrual cycle. Every month, a woman’s brain sends hormonal signals to the ovaries to produce different hormones at different times. The first half of the menstrual cycle is dominated by the hormone estrogen. It has effects on both the uterus & the ovaries. In the uterus, it will help the lining to grow thick in preparation of getting pregnant and having a soft place for the baby to implant. In the ovary, estrogen is responsible for telling multiple eggs every month to prepare themselves. These microscopic eggs will start to swell and when that happens we call them a follicle. One will become the winner also known as the “dominant follicle”. Around day 14 of the menstrual cycle, this dominant follicle will rupture, releasing the egg into the fallopian tube then the uterus. If you are sexually active and time intercourse appropriately, the egg can fertilize, and you can become pregnant. If you are not sexually active, the egg will continue through the uterus and exit a woman’s body. At the time of ovulation, a different signal from the brain tells the ovary to start making the hormone progesterone, which is the dominant chemical in the second half of the menstrual cycle. Progesterone will tell the lining of the uterus that it is no longer needed and will trigger shedding which we call a “period”. Progesterone also tells the ovaries that the remaining follicles are no longer needed, and they dissolve. WHAT HAPPENS IN PCOS? In a patient with PCOS, for multiple reasons, hormones and chemicals are “off” and while many eggs may start preparing themselves and turn into follicles, they never grow to any significant size and one does not become dominant or ovulate. If a woman doesn’t ovulate, she will not trigger progesterone and will not have shedding or bleeding. Essentially, women with PCOS are always in the first half of the menstrual cycle. They make many follicles, and the lining of the uterus grows thicker and thicker. But ovulation and menstruation do not occur. Eventually, the lining of the uterus become so thick that the body cannot hold onto it anymore. It will decide to release part of this tissue at random times. Not all of the lining will release at the same time. This is what is responsible for irregular vaginal bleeding. And because there’s so much extra tissue in there from months and months of accumulation, the bleeding is often quite heavy and prolonged… sometimes lasting more than 10 days or even two weeks. Most women with PCOS incorrectly believe that this is a “period”. This bleeding however is not a period, since ovulation did not occur. Instead, we refer to this as “withdrawal bleeding”. This irregular and heavy bleeding is more than just an inconvenience. While PCOS does not have any immediate dangers, there are some long-term consequences associated with it. WHAT ARE THE RISKS OF PCOS? Whenever there is tissue growth, there is always a chance that a “bad cell” appears. Typically, in women having regular periods once per month, the lining of the uterus sheds so frequently that any potential bad cells exit the body before causing problems. In women with PCOS however, the uterus does not shed each month. Thus, if there is a bad cell present, it can be retained for months or even years. Overtime, that cell can turn into a pre-cancer and eventually a cancer. So patients with PCOS are at increased risk of uterine cancer. But there is no reason to panic! There are ways to treat PCOS by regulating your hormones and having bleed each month. We achieve this by using birth control, most commonly pill. This will help your body have the appropriate amounts of both estrogen and progesterone at the right times each month and allow you to have regular withdrawal bleeds. Many women with PCOS like not having a period, and if you’re one of them don’t worry! There is a way to help regulate your hormones, and prevent the lining from growing too thick and causing a cancer, without having to bleed each month. We can do this within an intrauterine device (IUD). This is a small T-shaped device that is placed inside the uterus. While your body is naturally making estrogen each day, the IUD releases a small amount of progesterone each day in the uterus. This prevents the lining from growth thick and placing you at risk. By not allowing the lightning to grow, the IUD essentially stops you from having periods. While this device is typically used to prevent pregnancy, it is a wonderful option for women who have heavy periods or at risk of uterine cancer. Another complication of PCOS the patient often visits her gynecologist for is “infertility”. Yes, it’s true that you cannot get pregnant if you’re not ovulating, but the ovary of a women with PCOS contains multiple immature follicles. That is where the name Polycystic Ovarian Syndrome comes from. All we need to do is help those follicles to grow and have one rupture and that is ovulation! So PCOS patients have fertility options. There are medications and treatments available that can achieve this goal. So if you have PCOS, have been trying to get pregnant, and haven’t been successful, please visit your OB/GYN and they can help. Women with PCOS often have unwanted hair growth which is related to the abnormal hormones and slightly higher level of testosterone. There are many ways to treat this without having to undergo painful plucking, waxing, or laser treatments. Typically, birth control pills, which will help regulate your cycle and prevent uterine cancer, will also lower your testosterone and reverse unwanted hair growth. Finally, patients with PCOS typically suffer from obesity and experience difficulty losing weight. There are complex chemical abnormalities in patients with PCOS, including sugar and insulin imbalances similar to pre-diabetes. This is what helps you gain weight and makes it difficult to lose weight. There are wonderful protocols in existence which can help your metabolism get back on track. In fact, when used correctly, these medications can help with weight loss! In women with PCOS, losing 5 to 10% body weight typically will correct hormone levels and restore the normal menstrual cycle, ovulation, and bleeding. WHAT SHOULD YOU DO NOW? If you believe that you have PCOS, please reach out to your OB/GYN… because they can help you feel better and keep you safe!

How is my due date calculated? Your due date is set as the date that you will be 40 weeks pregnant. Initially, it is based on the first date of your last menstrual period. Some women have irregular cycles, do not know when their last period was, or have fluctuations in their cycle length. To ensure the correct due date, an initial ultrasound will be performed which will confirm or change your date. Will my due date ever change? Once your first ultrasound is performed, your due date will be set and this will not change. The earliest ultrasound is the most accurate so any subsequent ultrasounds will not alter your due date. However, there may be circumstances where certain medical conditions require delivery to occur at an earlier date. While that may be planned for you based on your individual situation, your “due date”will not change. (For example, repeat c-sections are typically performed at 39 weeks.) Can I have my baby on a specific date? While many people want to have (or avoid having) their baby on a certain date, in an effort to prevent complications to babies born prior to full term (39 weeks), hospital and medical governance boards have strict policies on timing of delivery. The American College of Obstetricians & Gynecologists (ACOG) provides guidelines regarding the timing of delivery. Elective (non-medical) deliveries prior to 39 weeks are not supported. Elective deliveries at or beyond 39 weeks are typically evaluated on a case by case basis and in accordance with hospital requirements. How many ultrasounds will I have? The American College of Obstetricians & Gynecologists (ACOG) recommends only one to two ultrasounds in pregnancy, however most OBGYNs will perform three. The first is typically done between 6 and 8 weeks to confirm that the pregnancy is inside the uterus, verify a heartbeat is present, and establish a due date. A second ultrasound is typically performed at 12 weeks to evaluate the nuchal translucency (NT) which is part of genetic screening as an increased thickness in the back of the baby’s neck may be associated with genetic abnormalities. A third ultrasound is performed around 20 weeks to look closely at the anatomy of the baby and ensure that it is normal. Additional ultrasounds may be recommended for certain medical problems or fetal growth concerns as necessary. Routine use of ultrasound for entertainment is not recommended by ACOG. When can I find out the gender? One of the most exciting parts of pregnancy is finding out if you are having a boy or a girl and planning on their arrival. Shopping for clothes, choosing baby items, and decorating a nursery are all part of the fun on welcoming a new member of your family. Some patients choose not to know the gender and wait for the “surprise” at delivery; others want to know as soon as they find out they are pregnant! Traditionally, the only way to determine gender was at the time of your 20-week anatomy ultrasound. This is still the standard way to find out what you are having. There are certain instances, however, where it may be recommended that patients have genetic testing performed on their pregnancy. Genetic testing will include an analysis of the sex chromosomes and as a result the gender will be known to your physician and can be shared.
Is my baby at risk? While most babies are born healthy, approximately 3-5% of babies are born with a birth defect. Some of these defects are caused by or associated with genetic disorders or syndromes. Some pregnancies are at increased risk of these birth defects or genetic disorders. These include mothers over the age of 35 at the time of delivery, a personal or family history of a birth defect or genetic disorder, and various other situations. What causes birth defects? Genetic disorders are caused by changes in a person’s genes or chromosomes. These changes are known as “mutations”. Aneuploidy is a condition where the chromosomes are off in number. If a chromosome is missing, it is known as monosomy; if there is an extra chromosome, it is referred to as trisomy. Trisomy 21 (or Downs Syndrome) is one of the most known aneuploidy conditions. Is genetic testing available for my baby? Historically, the only way to determine if a baby was at risk of genetic abnormalities was based on certain findings (known as “markers”) seen on the 20-week anatomy ultrasound. By this point in time, parents who were given bad news were faced with limited options as state termination laws generally prohibit ending a pregnancy beyond 20-24 weeks. Modern medicine recognized this problem and worked to develop testing methods which were more accurate and performed sooner, affording parents more time to decide what course of action was best to take given their individual situation. Various types of genetic testing have been developed including both screening tests and diagnostic tests. These can identify genetic abnormalities only, not structural abnormalities. What is a prenatal screening test? Prenatal screening tests can tell you the chances that your baby has an aneuploidy; it does not confirm a diagnosis and it may include false-positive (a positive result when the baby is actually normal) or false-negative (a negative result when the baby is actually affected) results. It includes lab tests performed during the 1st and/or 2nd trimester (depending on which test is used) and ultrasounds performed at 12 weeks and 20 weeks. The most accurate test is called cell-free DNA testing. It is a non-invasive prenatal test where genetic analysis is performed on some of the baby’s cells which are floating in mom’s blood. This test was designed for high risk patients but may be offered to all. There may be a cost associated with these tests. If positive results are encountered, patients will then be referred to have diagnostic testing performed to confirm the results. What is a prenatal diagnostic test? Prenatal diagnostic tests can tell you whether or not your baby actually has a genetic abnormality. These tests are done on cells from the placenta (chorionic villus sampling) or the amniotic fluid (amniocentesis). Chorionic villus sampling (CVS) is a diagnostic test performed during the first trimester (between 10-13 weeks of pregnancy) to determine whether or not a baby has a normal number of chromosomes. CVS is performed by inserting a core needle through a mother’s abdomen, into the uterus, and removing a small piece of the placenta. This tissue is analyzed in a laboratory and genetic testing is performed. The risk of miscarriage after CVS is approximately 1 in 250. Amniocentesis is a diagnostic test to determine whether or not a baby has a normal number of chromosomes. It is typically performed during the second trimester (between 15-18 weeks of pregnancy) but can be performed all the way up to the time of birth. An amniocentesis is performed by inserting a very thin needle through a mother’s abdomen, into the uterus, and withdrawing a small amount of amniotic fluid. Floating in that fluid are some of the baby’s cells that have naturally fallen off. These cells are then used by the laboratory for genetic testing. The risk of miscarriage after an amniocentesis is 1 in 1000. What is carrier screening? While prenatal genetic testing is concerned with the genes of the baby, carrier screening analyzes the genes of the mother and/or father to determine whether or not they have any unknown genetic abnormalities which can pass to their child and cause a disorder. Normal humans have two copies of every gene. For certain genetic disorders to occur, a person with that disorder must have two damaged copies of the same gene. As long as a person has at least one working copy of the gene, he or she is normally healthy and usually has no signs or symptoms of the genetic disorder. People who have one working copy and one damaged copy are called “carriers”. It is estimated that we all “carry” at least 8-10 of these damaged genes in our DNA. While having only one damaged gene doesn’t matter to us, if we have children with someone who also carries a damaged copy of the same gene, these children are at increased risk for having the genetic disorder. Who can have carrier screening performed? Carrier screening is offered to all people who are pregnant or planning on becoming pregnant. Because people of certain ethnicities are more likely to be carriers of certain disorders, most carrier screening is offered based on the ethnicity of you and the father of the baby. Some of the common genetic disorders screened for are cystic fibrosis (CF), fragile X, spinal muscular atrophy, (SMA), sickle cell anemia, and Tay Sachs disease. There are often no cures or treatments for these disorders. A baby can only be affected if both parents are carriers, and even then it is only a 25% risk the child will be affected. How is carrier screening performed? Carrier screening is done through a blood test on the female partner first. If the test result shows that the female partner is not a carrier, then no additional testing is needed. If the test result is positive, then the father of the baby is tested. The results of a carrier screen do not change from pregnancy to pregnancy and therefore mothers only need to be tested once time. (This is in contrast to genetic testing which is baby-specific to each pregnancy). Should I have testing in my pregnancy? It is a personal decision on whether or not to have genetic testing or carrier screening. Your individual beliefs and values are important factors in this decision. Some women make these decisions based on whether or not the results would change their plans to continue the pregnancy. Others choose to have testing while planning to continue their pregnancy no matter what, because they want time to possibly prepare for having a baby with a genetic disorder. Some want testing as reassurance on the likely positive outcome. Other parents do not want to know any information before the child is born and decide not to have testing at all. Financial considerations and support resources may also influence a family’s decision on whether or not to have testing performed. There is no right or wrong answer. Certain tests can only be done at certain times in pregnancy and tests performed earlier allow parents more time to make decisions if a result is positive. If ending the pregnancy would be considered, it is safest to do so within the first 13 weeks of pregnancy.

In the past, it was believed that once a woman had a cesarean section (c-section), all her future pregnancies would require the same delivery method. However, medical advancements have now made it possible for many women to attempt a vaginal birth after cesarean (VBAC). This article will explore the benefits, risks, and factors that determine whether a VBAC is a suitable option for you. What is a VBAC? A VBAC is a vaginal delivery after a woman has previously had a c-section. Vaginal births offer numerous advantages, including: Faster recovery times Shorter hospital stays Reduced risk of complications Lower rates of NICU admissions for the baby Decreased infection rates Lower rates of postpartum hemorrhage Who is a candidate for a VBAC? The American College of Obstetricians & Gynecologists (ACOG) has established guidelines to help determine which women can safely attempt a trial of labor after a c-section. Generally, women who meet the following criteria may be eligible for a VBAC: One or two prior c-sections with a horizontal incision on the uterus No previous uterine surgeries involving vertical incisions (such as those performed for premature babies under 28 weeks or myomectomy surgeries to remove uterine fibroids) No history of uterine rupture At least 9 months between the previous c-section and the current conception Risks associated with VBACs: While VBACs are generally considered safer than repeat c-sections, there are still some risks to be aware of. The most significant risk is uterine rupture, which occurs in less than 1% of women attempting a VBAC. Uterine rupture is a serious complication where the previous c-section scar opens during labor, potentially leading to life-threatening consequences for both mother and baby if not promptly addressed. This risk is highest in rural hospital settings with limited staff support or experience. Success rates of VBACs: Studies have shown that 60-80% of women who attempt a VBAC achieve a successful vaginal delivery. Factors that influence the likelihood of success include: Reason for the previous c-section: Women whose first c-section was due to a breech baby or concerns with the baby's heart rate during labor have a higher chance of success compared to those whose cervix stopped dilating or the baby never descended during pushing. Previous vaginal delivery: Women who have had a successful vaginal delivery in the past are more likely to have a successful VBAC. Timing of labor: The highest success rates for VBACs occur when women go into labor spontaneously before 40 weeks of pregnancy. After 40 weeks, the chances of a successful VBAC decrease. If you're considering a VBAC for your next pregnancy, the experienced team at Alliance Obstetrics & Gynecology, LLC is here to support you. Our skilled obstetricians will work closely with you to determine whether a VBAC is a safe and appropriate option based on your individual medical history and current pregnancy. We prioritize personalized care and support throughout your pregnancy journey, ensuring you have the information and resources needed to make informed decisions about your delivery. Contact Alliance Obstetrics & Gynecology, LLC today to schedule a consultation and learn more about your options for a successful VBAC. If you have had a previous c-section and are considering a VBAC for your next pregnancy, it is essential to discuss your options with your healthcare provider. They will assess your individual circumstances, including your medical history and current pregnancy, to determine whether a VBAC is a safe and appropriate choice for you. Remember, every pregnancy is unique, and the decision to pursue a VBAC should be made in collaboration with your medical team, taking into account your personal preferences and health status.



